Lupus Nephritis
New intervention targets T cells rather than multiple immune cell types
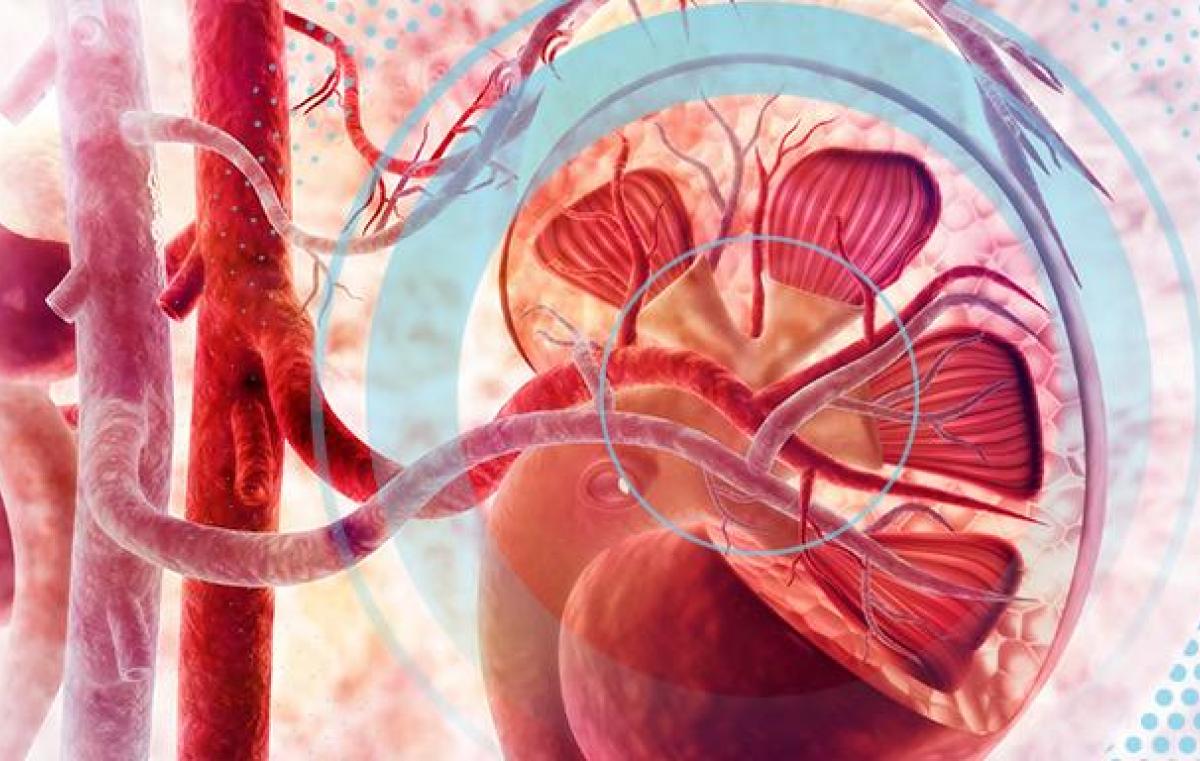
Lupus (systemic lupus erythematosus), an autoimmune disease in which the body recognizes and attacks its own tissues, can affect many organs, including the kidneys. About fifty percent of patients diagnosed with lupus develop lupus nephritis, which is inflammation that can destroy the kidneys, among the most vital organs in the body.
Several medications currently available can effectively treat lupus nephritis, but in patients who don't respond well to these treatments, the disease can progress to such an extent that the only way to keep them alive is through dialysis or a kidney transplant. Additionally, most of these medications can cause many side effects, including suppression of the immune system and an increased susceptibility to infections.
A new, targeted therapy, developed by researchers from the Azrieli Faculty of Medicine of Bar-Ilan University, the Albert Einstein College of Medicine, the University of Houston, and the pharmaceutical company Equillium, together with several other academic collaborators, inhibits specific immune cells associated with lupus nephritis, and was effective in improving kidney inflammation in animal models of lupus and lupus nephritis. The new approach could serve as an alternative to current treatments targeting multiple immune cells, and provide a more effective and potentially personalized remedy for lupus nephritis. The development was reported in a study published today in the Journal of Clinical Investigation.
Many different types of immune cells are involved in the mechanisms underlying target organ damage in lupus and other autoimmune conditions. One of these important cell types is T-cells, which affect the kidney by interacting and binding with other cells, much like a key inserts into a lock. T-cells expressing CD6 (the lock) bind with a molecule known as ALCAM displayed on other cells (the key) causing T-cell activation which leads to kidney inflammation. To prevent this damaging development, the researchers developed an antibody that disrupted the process by blocking the interaction between CD6 and ALCAM, just as glue in a lock would prevent a key from being inserted into it. As a result, T-cells didn't get activated. Indeed, when activation of the CD6/ALCAM pathway was blocked in animal models, the researchers observed significant therapeutic improvement in kidney inflammation.
"Up until now, CD6/ALCAM interactions weren't considered relevant or instrumental in lupus nephritis," says Prof. Chaim Putterman, of the Azrieli Faculty of Medicine of Bar-Ilan University (Safed, Israel) and the Albert Einstein School of Medicine (Bronx, NY), who led the study together with senior co-authors Dr. Cherie Ng and Dr. Chandra Mohan. "The intervention we describe, which targets T cells rather than multiple immune cell types, can potentially provide physicians with another effective tool for treatment of a difficult and challenging disease."
In a separate experiment, the researchers detected elevated levels of ALCAM molecules in urine samples of lupus patients with kidney inflammation, and discovered additional evidence for the activation of the CD6/ALCAM pathway in human lupus kidneys. The finding that ALCAM is elevated in the urine suggests a potential new path toward personalized medicine. The researchers believe that if they can develop the anti-CD6 antibody to treat patients with lupus nephritis, it might work best on those patients with high urine ALCAM, as these are the patients who should be most amenable to blockade of the CD6/ALCAM pathway. Ongoing clinical trials will determine whether these findings lead to therapeutic benefit for humans.
Image: (c) 2022 American Society for Clinical Investigation